SARS-CoV-2 (Severe acute respiratory syndrome coronavirus 2 – the virus that causes COVID-19) persistence in metalworking fluids
Does the SARS-CoV-2 virus persist in Water-Miscible Metalworking Fluids?
Over the past two months, I have received quite a number of emails and phone calls asking if water-miscible metalworking fluids (MWFs) were likely to be a source of SARS-CoV-2 virus exposure for machinists and others working in machine shops.
My short answer is that nobody really knows. I know that this answer is not particularly reassuring, but the test methods needed to test MWFs and MWF mists for SARS-CoV-2 in there types of samples do not yet exist. For companies and institutions developing test methods to detect SARS-CoV-2 the first priority has been identifying infected individuals. Given that most transmission seems to be via inhalation of aerosol droplets that carry virus particles, and that the aerosols of primary concern are those produced when someone sneezes, coughs, or speaks, investigating virus persistence in fluids was initially considered to be a less critical need.
However, for those working in the manufacturing sector, there is a history of adverse health effects – primarily allergies – caused by MWF aerosol exposure. Also, COVID-19 can be transmitted by touching a SARS-CoV-2 contaminated surface (i.e., contaminating the hands with viruses) then bringing the hands to the face. The virus can then be inhaled or gain entry through the eyes. If SARS-CoV-2 persists in MWFs, then machinists whose hands are in contact with the fluid and who then touched their face are at increased exposure risk. Additionally, machinists handle the parts that are to be machined. According to the European Centre for Disease Prevention and Control, SAR-CoV-2 an persist on copper surfaces for up to 4h, cardboard for 24h, and plastic or steel surfaces for up to three days. This means that there are ways COVID-19 can be transmitted at metalworking facilities.
Can we reasonably use what we know to assess the risk?
I believe that we can use the guidance provided by the Centers for Disease Control, (CDC) to minimize the incremental risk to machinists. Note that I am addressing incremental risk – that is the risk over and above our risk of contracting COVID-19 from our other activities. We are all at risk, however, all of the epidemiological studies that have been reported to date agree that social distancing reduces risk. To understand the incremental risk, we need to understand a few concepts:
Risk
Risk is a function of hazard + exposure (R = H + E – Figure 1). This means that the most hazardous substance poses no risk if exposure is zero. All of the clinical and epidemiological studies that have been published since the first reports of COVID-19 in Wuhan, China last November indicate that SARS-CoV-2 virus is quite hazardous. Although the number of virus particles needed to cause a COVID-19 infection is not known, the ease with which the disease spreads from infected individuals to susceptible victims, the severity of many non-lethal infections, and apparent mortality rate (percentage of people who have contracted clinically reported infections and who ultimately die from the disease) demonstrate that SARS-CoV-2 is hazardous. Consequently, until a SARS-CoV-2 vaccine is developed, the primary means of reducing disease risk is isolation.
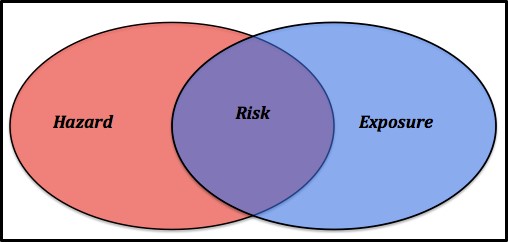
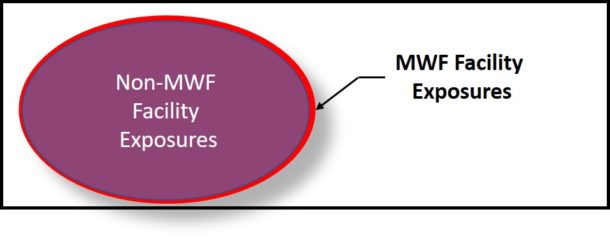
In many respects, the risks encountered at manufacturing facilities are identical to those related to the general population’s activities. For example, most people walk outdoors, handle doorknobs, groceries, appliances (computer, TV, smart phones, etc.), and generally expose themselves in countless ways. As depicted in Figure 2, this (blue ellipse) is our non-MWF facility exposure. For those who work at manufacturing facilities, there is some incremental exposure (red ellipse in Figure 2). Note, this is not to scale. We do not know the actual incremental risk.
Acceptable Risk
Risk is an objective concept. You can compute it if you know the hazard and the exposure (direct contact). Acceptable risk is purely subjective. The chances of dying in a plane crash are 1 in 11 million (0.000009 %) and of dying in a bathtub are 1 in 840,000 (0.0001 %). However, fear of flying represents an unacceptable risk to more people than fear of bathing does. Throughout the world today, we see the impact of differing opinions regarding risk acceptability playing out. At one extreme, people have placed themselves in complete isolation. At the other, people are ignoring all COVID-19-related personal hygiene and social distancing guidance. There is no broad consensus on the appropriate balance between measures to reduce the exposure risk and those taken to sustain the economy. One both sides of the argument, hysteria tends to take precedence over objective risk assessment. Intelligent, honest people can reasonably disagree on what constitutes an acceptable SARS-CoV-2 exposure risk. I will steer clear of that argument here but will note that as the COVID-19 pandemic has illustrated, risks rarely exist in isolation. Reducing one risk can easily increase another risk. In the case of COVID-19, decreasing the disease risk has increased the poverty risk for many people.
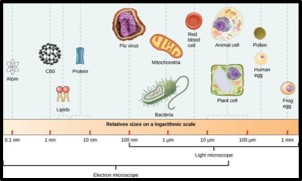
Viruses
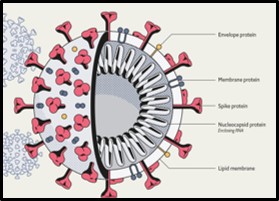
Viruses are sub-microscopic (i.e., can been seen through an electron microscope but are too small to be seen through a light microscope – as seen in Figure 3, viruses are ∼0.001 times the size (volume) of bacteria and ∼0.000001 times the size of human cells). They contain genetic material enveloped in a coat. More than 6,000 different viruses have been identified (no doubt a tiny fraction of the different types of viruses that exist). Some – including SARS—CoV-2 – contain ribonucleic acid (RNA) and others contain deoxyribonucleic acid (DNA) as their genetic material. Virus coats can be protein or protein and lipid (Figure 4 shows the SARS-CoV-19 structure). Viruses can persist (i.e., remain infectious) but cannot multiply outside of susceptible (host) cells. Most viruses can only attack specific types of cells. The infection process starts with one or more viruses attaching to sites on the host’s cell wall. For SARS-CoV-2 viruses, the spike protein attaches to a cell. The virus then injects its genetic material into the host cell and the virus’ genes hijack the host cells’ genes – redirecting them to produce new viruses. Once the host cell is full of newly manufactured virus particles, it breaks open (lyses) to release the viruses into the environment surrounding it. If there are no susceptible cells to infect, a virus will eventually decompose. This is the basis for the persistence testing. When 3 days persistence is reported, that means that although the number of infectious viruses is decreasing from the moment they are deposited onto a surface, it takes 3 days for the number has decreased to below the test method’s detection limit (the detection limit is the minimum number/value that can be measured by a given test method).
Detecting viruses
Viruses are cultured by inoculating a layer of susceptible cells (i.e., a tissue culture) with a specimen containing viruses. As they infect the tissue culture cells, the viruses create clear zones – plaques – each of which contains billions of individual virus particles – virions (Figure 5). Viruses isolated by culture testing can then be used to develop other test methods. The most common methods are immunoassays (detect the presence of antibodies to specific viral antigens) and genetic tests (see my January 2018 What’s New posts for more detail explanations of antigen and genetic test methods).
At present the lower detection limit for SARS-CoV-2 virions is ∼2,700. A sneeze droplet from an infected person can carry millions of virions. That makes it relatively easy to detect the virus on contaminated surfaces or on a nasal swab sample. If that same sneeze droplet lands in 1 mL of fluid, the number of virions in that droplet are diluted 50,000-fold. As the ratio of the fluid volume into which someone has sneezed, coughed, etc. increases, so does the dilution factor and the difficulty of detecting viruses in the contaminated fluid. Consequently, to be detected in fluids (water, MWF, etc.) virus particles must first be concentrated. This concentration step is easier with fluids that have few contaminants (for example, potable water) than with complex, contaminant loaded fluids like MWFs. Consequently, it might be months or years before methods are developed to detect and quantify SARS-CoV-19 virus particles in MWFs.
Risk Assessment
Clearly, without data, assessing the risk of COVID-19 infection due to exposure in metalworking facilities is an exercise in speculation. However, because of the pandemic-related epidemiological studies that have been done for the general public and at food processing facilities, there is a basis for an educated guess.
Bioaerosol Exposure
Social distancing is the most effective way to reduce exposure. The general CDC guidelines apply equally well to personnel working in machine shops. Although mist collection systems have reduced MWF mist exposure, and the incidence of reported clusters of industrial asthma and other respiratory diseases has plummeted since the 1990s, when mist collection systems were installed at many metalworking facilities, there remains some question about how well mist collectors capture sub-micron diameter, bioaerosols. It is likely that there remains some risk of bioaerosol exposure, but there are insufficient data to define that risk. Generally speaking, recirculating MWFs act as bioaerosol reservoirs (i.e., the source) and MWF system biofilms act as MWF microbial contamination reservoirs. There have not been any reported studies of virus loads in MWF aerosols or virus presence or persistence in MWFs, so it is difficult to predict SARS-CoV-19 persistence in MWFs.
Some studies have been done to evaluate the COVID-19 risk to wastewater treatment plant operators. It has been reported that SARS-CoV-19 can persist for “2 days at 20°C, at least 14 days at 4°C, and survive for 4 days in diarrheal stool samples with an alkaline pH at room temperature.” (source: https://www.waterra.com.au/_r9550/media/system/attrib/file/2200/WaterRA_FS_Coronavirus_V11.pdf). Given that MWFs are alkaline and that the temperature of recirculating MWFs typically ranges between 30 °C (86 °F) and 37 °C (100 °F) it is likely that the virus will persist for 2 to 7 days in MWFs. Consequently, there is a risk that workers can be exposed to virus particles in MWF mist droplets.
Contact exposure
As noted above, the SARS-CoV-2 virus can persist on steel surfaces for up to 3 days. Consequently, handling parts that have become contaminated with virus particles within the previous 3 days poses an infection risk.
Risk Mitigation
Social distancing
Workers are typically standing shoulder to shoulder at food processing facilities where COVID-19 clusters have been reported. The distance between machines at metalworking facilities is more conducive to social distancing. Keeping at least 1.8 m (6 ft) distance between workers substantially decreases the risk of transmission among workers.
Mist control
Reduced mist exposure translates to reduced risk. If enclosures remain closed for at least 30 sec after MWF fluid flow is stopped, then the risk of mist inhalation decreases substantially. Equally important is mist collection system maintenance. To operate effectively, mist traps and reservoirs must be kept clean. Their surfaces should be disinfected after each leaning. High-efficiency particulate air (HEPA) filters installed at mist collect exhausts must be changed with sufficient frequency to prevent filters from becoming a source of bioaerosol exposure. Effective facility ventilation – including air flow and relative humidity control – will reduce virus persistence.
Personal protective equipment (PPE)
The role of appropriate PPE, properly worn and maintained, in preventing respiratory disease and dermatitis has been well documented. Workers likely to be exposed to MWF aerosols should wear air filtration masks that will prevent virus inhalation (i.e., meet or exceed capabilities of N-95 masks). Other masks help to remind individuals not to touch their face and trap aerosol droplets that they produce but do little to prevent them from inhaling virus particles that are in the air. Non-porous gloves can prevent direct contact with viruses that are on part surfaces. However, surgical gloves are likely to tear quickly when used to handle tools, machines, and parts. Recognizing that SARS-CoV-2 particles can persist on glove surfaces for several days, it is important to disinfect gloves with a hand sanitizer before removing them.
Personal hygiene
It seems that a substantial percentage of people with COVID-19 infections never show symptoms. However, these individuals can infect others. Effective personal hygiene practices can mitigate the disease transmission risk. Effective measures, as detailed by the CDC (see link above) include keeping hands away from the face and washing hands frequently – after each time a person touches any surface that might be contaminated with the SARS-CoV-19 virus. Applying a hand sanitizer can be an effective alternative to constant washing. The standard metalworking facility personal hygiene practices that have been advocated for decades also apply here. Workers should wear clean shop clothes. Street cloths should no be worn in the metalworking facility and work cloths should be cleaned by an industrial laundry service. Personnel should not eat, drink, or smoke before having washed hands thoroughly. Individuals should wash hands both before and after using the lavatories.
Bottom Line
Because workers are exposed to MWFs and parts, there is some incremental risk of SARS-CoV-2 exposure associated with working at metalworking facilities. Given that in contrast to food processing facilities there have been no reported COVID-19 clusters at machine shops, the incremental risk is likely to be small. Still, there are steps that owners, managers, and workers can take to minimize workplace-related incremental risk. Taking these measures can help maintain productivity while protecting workers from unnecessary COVID-19 risk. From the moment of birth to the moment of death, our lives are risk-laden. It is impossible to reduce risk to zero. However, by remaining mindful of potential sources of exposure and taking precautions to avoid bioaerosol inhalation, metalworking industry stakeholders can minimize the risk of workplace exposure.
Stay safe, productive, and healthy! Please send your comments and questions to me at fredp@biodeterioration-contol.com.